The Reality of Inpatient Psychiatric Work Today

Inpatient psychiatry has always been an intense, high-pressure environment where clinicians must make crucial decisions quickly, often with limited information. Patients admitted to psychiatric units tend to present with high acuity symptoms—such as psychosis, mania, suicidal ideation, aggression, or severe withdrawal—requiring rapid assessment and stabilization. Psychiatrists must manage these crises while also coordinating with nursing teams, social workers, internal medicine, and hospital administration. Each decision carries significant clinical, legal, and safety implications. The workload is further complicated by the unpredictable nature of psychiatric admissions, fluctuating census numbers, and the ever-increasing complexity of patient presentations.
Compounding these challenges is the substantial administrative burden placed on clinicians. Admission notes, daily progress documentation, medication rationale, legal paperwork, treatment plans, and discharge summaries consume several hours each day. Much of this documentation is repetitive or clerical in nature, yet essential for regulatory compliance. As a result, psychiatrists often struggle to dedicate sufficient time to direct patient care because they must focus heavily on meeting documentation requirements. With rising patient loads and national staffing shortages, the strain on inpatient psychiatrists has become more severe than ever. This is where Co-Pilot psychiatric decision support can dramatically change workflow efficiency, improve accuracy, and enhance patient outcomes.
High acuity, polypharmacy, and documentation overload

Inpatient psychiatric units frequently manage patients with multiple psychiatric diagnoses, chronic medical illnesses, and extensive medication histories. Polypharmacy is not only common—it is often unavoidable. Patients may arrive on complex combinations of antipsychotics, mood stabilizers, antidepressants, benzodiazepines, and medical medications. Determining what to discontinue, what to continue, and what to adjust is a time-sensitive task that requires deep clinical knowledge and careful review. Missing a drug interaction, duplicating therapy, or misunderstanding a patient’s medication history can lead to serious consequences.
Documentation adds another layer of pressure. Each patient requires thorough, legally compliant notes every day. Psychiatrists must explain medication decisions clearly, justify level of care, address safety concerns, and communicate with the treatment team. Many clinicians report spending more time documenting than interacting with patients—an imbalance that affects both clinician satisfaction and patient care quality. Co-Pilot can significantly reduce these burdens by analyzing patient histories, flagging medication risks, generating detailed clinical notes, and helping prioritize clinical tasks. With Co-Pilot support, psychiatrists can focus more on treatment and less on paperwork.
What Is Co-Pilot Psychiatric Decision Support?

Co-Pilot psychiatric decision support refers to advanced, data-driven tools that help clinicians make faster, safer, and more informed decisions. These tools analyze clinical data—symptoms, medication lists, histories, lab results, imaging, and patient-reported information—to offer evidence-based recommendations. They do not replace clinicians; rather, they enhance clinical judgment by sorting through vast amounts of information instantly.
In the inpatient psychiatry setting, Co-Pilot can solve several major challenges. It can rapidly compile fragmented data from previous hospitalizations, summarize complex medical histories, flag medication interactions, and predict potential clinical risks. Co-Pilot tools equipped with natural language processing can also generate drafts of admission notes, progress notes, and discharge summaries. This supports clinicians by reducing the time spent on repetitive tasks while increasing accuracy. As the demand for inpatient psychiatric care continues to rise, these tools are becoming essential components of modern clinical practice.
Core capabilities (diagnosis support, meds, documentation)

Co-Pilot psychiatric decision-support systems typically offer three primary capabilities:
Diagnostic support
Co-Pilot reviews symptoms, timelines, comorbidities, past diagnoses, and medical data to suggest possible differentials. For new admissions with unclear histories, this feature can significantly speed up diagnostic formulation.
Medication and treatment guidance
Using clinical guidelines, population-level treatment data, and medication interaction databases, Co-Pilot can provide evidence-based medication suggestions. It also identifies safety risks, duplicate therapies, metabolic concerns, QT prolongation risks, and interactions with medical medications.
Documentation assistance
Co-Pilot can draft structured documentation including admission notes, progress notes, treatment plans, and discharge summaries. Clinicians simply review and edit as needed. This reduces hours of writing and ensures consistent, compliant documentation.
Top Use Cases on Inpatient Units
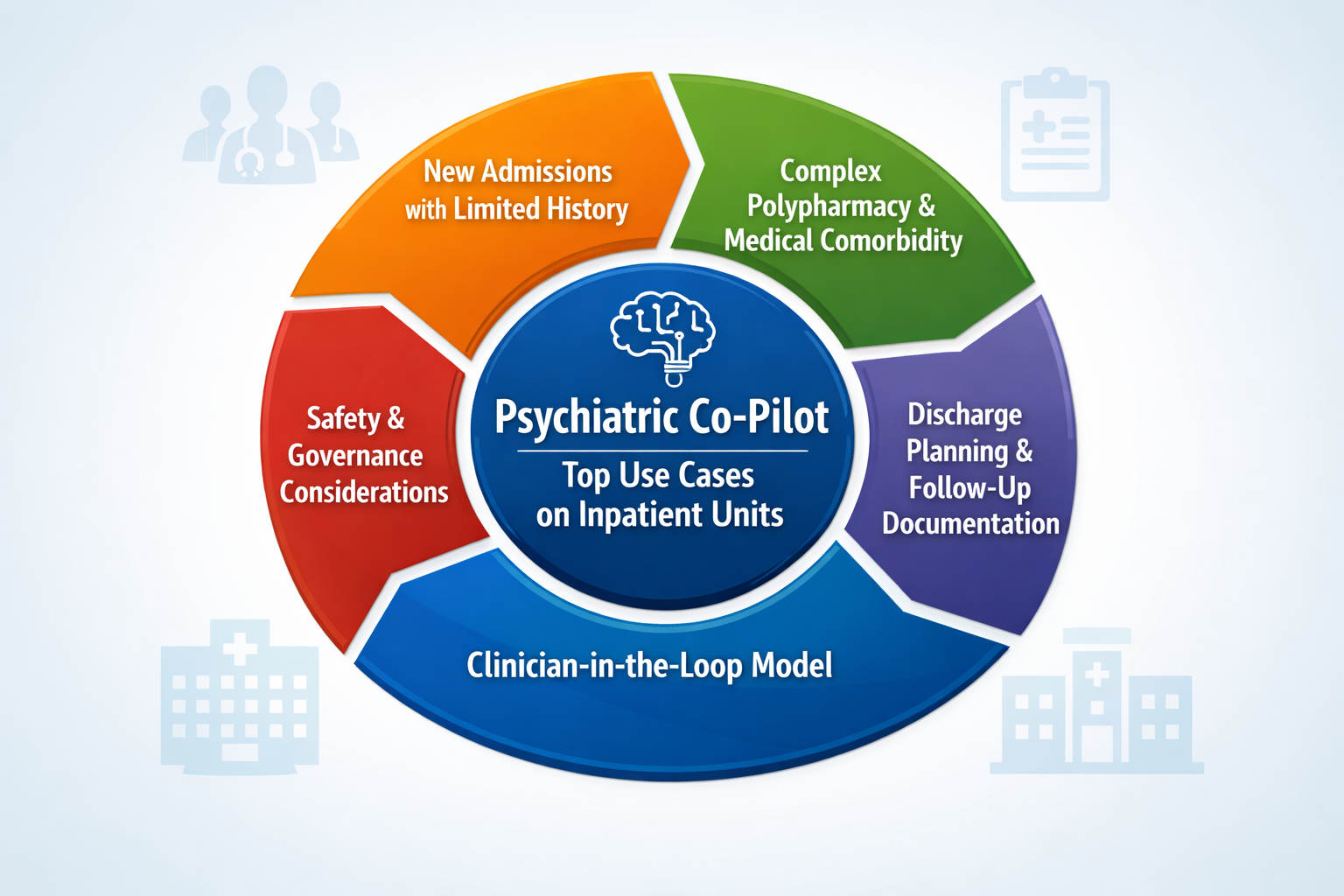
Co-Pilot psychiatric decision support is especially powerful in inpatient settings where clinicians face time-critical decisions and unpredictable workloads. Below are the areas where Co-Pilot delivers the greatest impact.
New admissions with limited history
New admissions are among the most challenging scenarios for inpatient psychiatrists. Patients may arrive agitated, confused, sedated, or unable to provide an accurate history. Co-Pilot can quickly analyze existing records, past hospitalization data, medication lists, and diagnostic patterns to create an organized clinical snapshot. This allows clinicians to stabilize patients more quickly and avoid delays caused by missing information.
Complex polypharmacy and medical comorbidity
Inpatient psychiatrists treat many patients with co-occurring psychiatric and medical illnesses. Conditions like diabetes, hypertension, renal disease, substance use disorders, and cardiovascular issues compound medication risks. Co-Pilot tools can cross-check all current medications, identify potential interactions, highlight medical contraindications, and recommend safer alternatives. This reduces the risk of medication errors—a common and serious issue in inpatient psychiatry.
Discharge planning and follow-up documentation
Discharge summaries are time-consuming but essential. They must include diagnoses, treatment courses, medication rationale, risk assessments, and follow-up plans. Co-Pilot dramatically simplifies this process by synthesizing clinical notes and progress data into a complete, accurate summary in seconds. This ensures patients receive consistent, high-quality discharge documentation and helps reduce the administrative burden on clinicians.
Safety and Governance Considerations
While Co-Pilot brings tremendous benefits, safety and governance must remain top priorities. Co-Pilot tools must adhere to health privacy laws, maintain accurate clinical logic, and operate within a framework that ensures responsible, clinician-supervised use. Hospitals should establish protocols for Co-Pilot adoption, including training, data governance, audit processes, and clear guidance on how AI-generated content is reviewed.
Co-Pilot should always be used to support—not replace—clinical expertise. In psychiatric care, where empathy, clinical judgment, and human understanding are essential, the clinician must remain the final decision-maker.
Clinician-in-the-loop model
The clinician-in-the-loop approach is the safest and most appropriate model for Co-Pilot in psychiatric care. The Co-Pilot generates recommendations or documentation drafts, and the clinician verifies and finalizes them. This protects patient safety, maintains clinical autonomy, and ensures that the Co-Pilot acts as a partner rather than a substitute. With the clinician in full control, the use of Co-Pilot becomes both safe and highly effective.
How OnDemand Psych Fits Into Inpatient Workflows

OnDemand Psych is uniquely designed for inpatient psychiatry and supports clinicians at every stage of the inpatient workflow. It provides real-time diagnostic suggestions, medication guidance, risk assessments, and auto-generated clinical notes. During morning rounds, OnDemand Psych can highlight overnight changes, summarize key risks, and assist with progress note creation. For admissions, it can build detailed note drafts instantly. For discharges, it can prepare summaries with all essential details.
Its medication decision-support engine is especially valuable for polypharmacy cases, offering clear guidance on interactions, side effects, and evidence-based treatment options. OnDemand Psych integrates smoothly with existing workflows, making it a powerful addition to any inpatient unit seeking efficiency, accuracy, and improved patient safety.
Getting Started With Co-Pilot on Your Unit
Integrating Co-Pilot psychiatric decision support on an inpatient unit begins with assessing workflow bottlenecks—whether it’s admissions, documentation, or medication management. Once priorities are identified, hospitals can begin with a phased implementation that allows clinicians to adopt the tool without disrupting existing operations.
Training sessions ensure clinicians understand how Co-Pilot works, how it supports clinical reasoning, and how to maintain a clinician-in-the-loop approach. Within a short time, most units report significant reductions in administrative time, improved diagnostic clarity, smoother medication management, and more consistent documentation. As inpatient psychiatry continues to evolve, adopting Co-Pilot tools is becoming essential for maintaining high-quality, sustainable care.
Conclusion
Co-Pilot psychiatric decision support has the potential to transform inpatient psychiatry by addressing some of its biggest challenges—complex cases, medication risks, documentation overload, and unpredictable patient flow. By supporting clinicians with diagnostic insights, medication safety tools, and automated documentation, Co-Pilot enhances patient care while reducing burnout. Platforms like OnDemand Psych demonstrate how Co-Pilot can fit seamlessly into inpatient workflows, improving safety, consistency, and efficiency. As mental health demands continue to rise, integrating Co-Pilot into inpatient psychiatry will become not just helpful but essential for delivering high-quality, reliable patient care.
FAQs
1. What is Co-Pilot psychiatric decision support?
It is a technology that analyzes clinical data to help psychiatrists make accurate, evidence-based decisions on diagnosis, medication, and documentation.
2. How can Co-Pilot help inpatient psychiatrists?
Co-Pilot reduces documentation time, identifies medication risks, summarizes complex histories, and supports diagnosis—allowing clinicians to work faster and more safely.
3. Does Co-Pilot replace clinical judgment?
No. Co-Pilot assists clinicians but does not replace their expertise. All decisions remain under clinician supervision.
4. Is Co-Pilot safe for inpatient psychiatric care?
Yes, when implemented with a clinician-in-the-loop model, strong governance, and validated clinical guidelines.
5. How does Co-Pilot help with polypharmacy?
Co-Pilot flags drug interactions, contraindications, and duplications, helping clinicians safely manage complex medication regimens.
6. How can inpatient units start using AI?
Units can begin by identifying workflow challenges, adopting a phased rollout, training clinicians, and integrating tools like OnDemand Psych.